The challenges of Medicaid re-enrollment and how state agencies can manage them
Millions of people have lost Medicaid coverage for administrative reasons, such as not having a current address on file or submitting an incomplete renewal application.
Many of those who’ve been disenrolled are seeking to re-enroll. But not all are eligible.
Download the full infographic ↗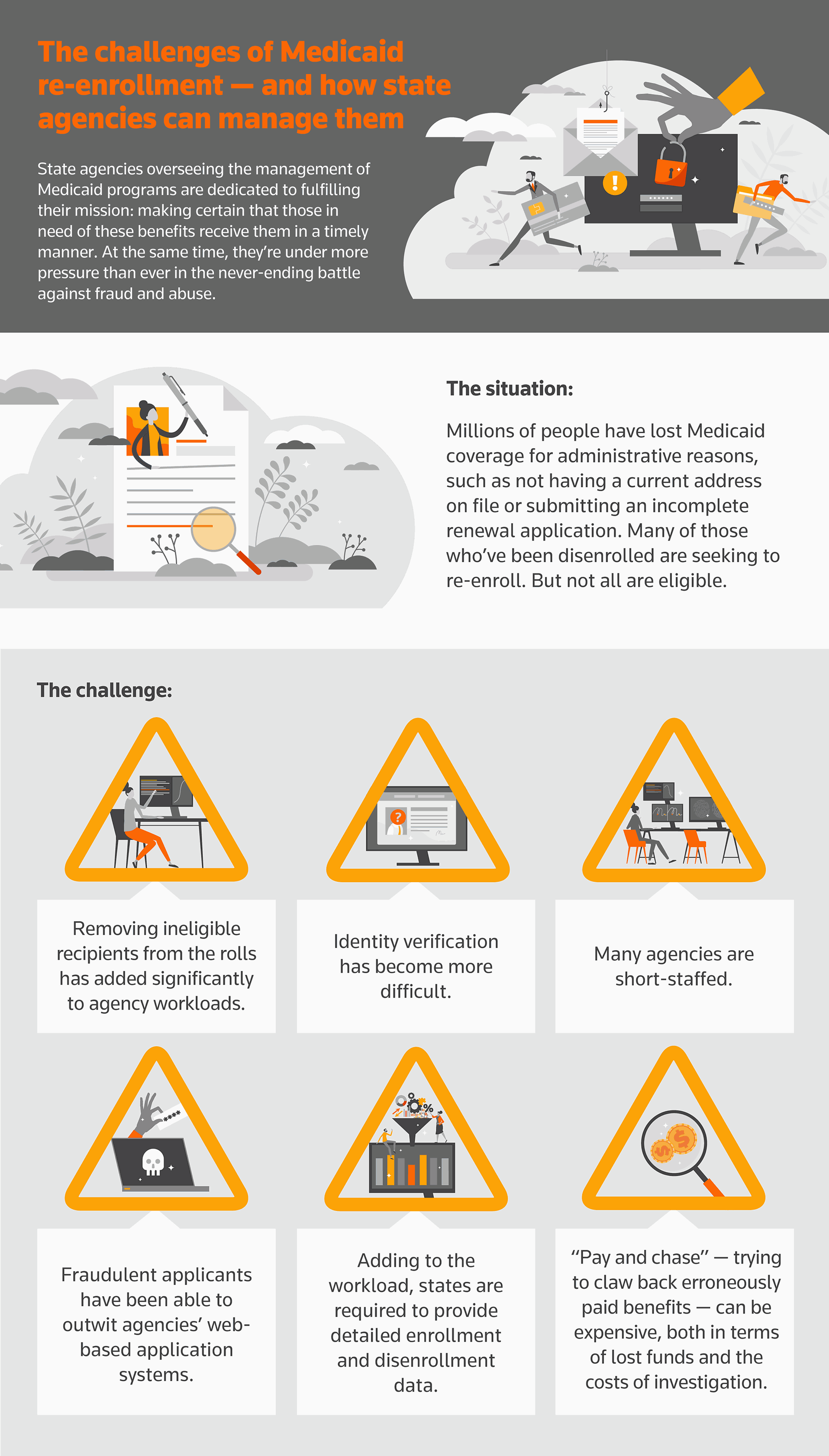
A proactive solution:
Seeking to be proactive about protecting Medicaid funds, agencies have begun using digital solutions for fraud prevention, detection, and investigation. These solutions are available either as software or through a service. According to Thomson Reuters research, the top reasons agencies choose software over a service include:
- The ability to manage and ensure data privacy and protection
- Cost-effectiveness
- The capability to analyze and monitor data in real time
State Medicaid agencies are exploring forward-thinking approaches to make sure those truly in need of Medicaid benefits receive them. Read the white paper State Medicaid agencies: New challenges in the battle against fraud to learn more.
 |
Thomson Reuters is not a consumer reporting agency and none of its services or the data contained therein constitute a ‘consumer report’ as such term is defined in the Federal Fair Credit Reporting Act (FCRA), 15 U.S.C. sec. 1681 et seq. The data provided to you may not be used as a factor in consumer debt collection decisioning, establishing a consumer’s eligibility for credit, insurance, employment, government benefits, or housing, or for any other purpose authorized under the FCRA. By accessing one of our services, you agree not to use the service or data for any purpose authorized under the FCRA or in relation to taking an adverse action relating to a consumer application.