Fraud detection software
Improve fraud detection and prevention with Fraud Detect
A powerful tool that utilizes expert machine-learning technology
Providing you with actionable, trusted analytics and results
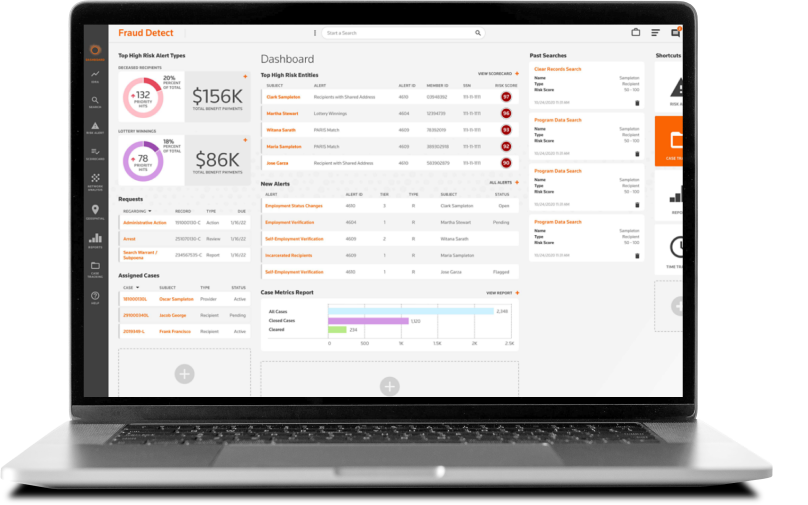
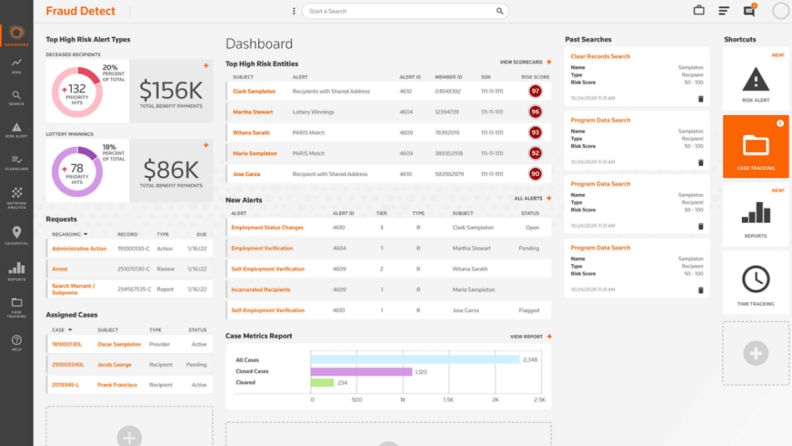
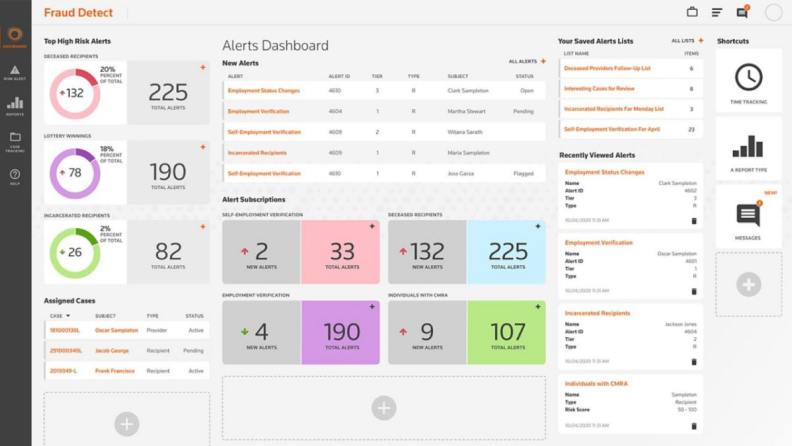
Detect fraud behavior patterns with confidence
Get detailed analyses to predict and detect complex schemes. You'll receive risk-scoring, stack-ranked lists of all program providers and participants based on their risk for fraud.
Explore more features
Have questions?
Contact a representative
Gain insightful analytics from advanced prediction and machine-learning technology
Discover potential fraud through trends, patterns, clusters, and individual leads. This information is delivered through easy-to-interpret graphs, link charts, tables, and other methods to clearly display the cause for suspicion.
Explore more features
Have questions?
Contact a representative
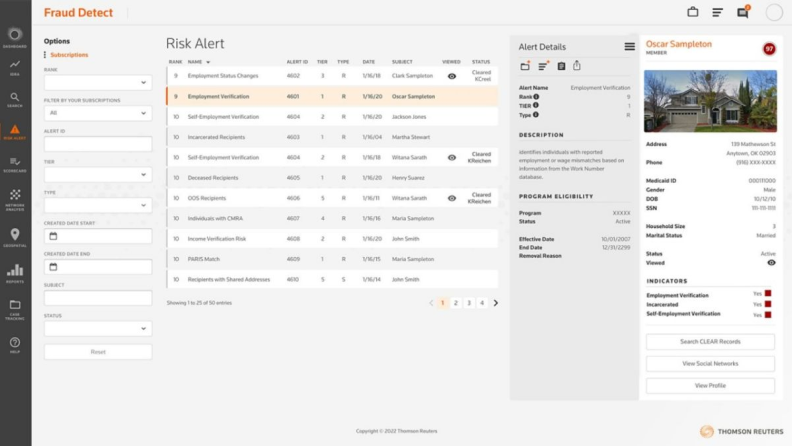
Prioritize investigation-ready leads with enhanced data
With the addition of CLEAR public records, your analysts and investigators are provided with enhanced program data containing live data updates that can highlight which leads should be prioritized.
Explore more features
Have questions?
Contact a representative
Fraud Detect can meet your industry-specific needs
Unemployment
Find fictitious businesses — and improper or overpayments — while keeping unemployment benefits in the right hands. Fraud Detect is critical to maintaining program integrity, verifying information, and ensuring risks are called to attention for action.
Social Services
Detect complex SNAP fraud schemes, get a comprehensive review of fraudulent patterns in SNAP programs, and reduce the amount of improper payments by detecting bad actors misusing or trafficking benefits.
Healthcare
Fraud Detect can help agencies comply with CMS regulations regarding fraud, waste, and abuse oversight and reporting by revealing unlicensed providers, outlier billing, utilization spikes, and much more.
The value of Fraud Detect
$18.7 million recovered
Fraud Detect identified $50 million in overpayments, which led to $18.7 million in recoveries by Medicaid Inspector General.
40% of top Medicaid states
Four of the top 10 Medicaid states are utilizing Fraud Detect to prevent fraud in their programs.
$130 million identified
The duplicate payment model identified $130 million in duplicate payments.
Questions about Fraud Detect? We’re here to support you.
972-998-0883
Call us or submit your email and a sales representative will contact you within one business day.
Contact us
Fraud Detect support
Get answers to your Fraud Detect questions
Thomson Reuters is not a consumer reporting agency and none of its services or the data contained therein constitute a “consumer report” as such term is defined in the Federal Fair Credit Reporting Act (FCRA), 15 U.S.C. sec. 1681 et seq. The data provided to you may not be used as a factor in consumer debt collection decisioning; establishing a consumer’s eligibility for credit, insurance, employment, government benefits, or housing; or for any other purpose authorized under the FCRA. By accessing one of our services, you agree not to use the service or data for any purpose authorized under the FCRA or in relation to taking an adverse action relating to a consumer application.